In many facets of life, doing something at a 70 percent completion rate is pretty good. But when it comes to vaccine deployment and administration, 70 percent isn’t good enough. As of Sunday, the U.S. has administered 41,210,937 doses of COVID-19 vaccines and distributed 59,307,800 doses. That’s good for about 70 percent.
Of the 41 million who have received the vaccine, only approximately 9 million have received both doses of either the Pfizer or Moderna vaccine. The Johnson and Johnson vaccine, which only requires one shot, was submitted for emergency use authorization last week and should help move along those numbers. Regardless, the country has a long way to go.
“This will be one of the most difficult operational challenges we’ve ever undertaken as a nation,” President Biden said during an interview with CBS News that aired before the Super Bowl. He predicted that because of manufacturing and operational challenges, it will be late Summer by the time the country could vaccinate 300 million people and reach herd immunity.
The original Operation Warp Speed goal, set by the Trump administration in mid-2020, was 300 million vaccinated by the end of January 2021. In a recent webcast hosted by the Alliance for Health Policy, James Blumenstock, Senior Vice President, Pandemic Response and Recovery, Association of State and Territorial Health Officials, said that there were a few reasons why that goal hasn’t been reached and why the country has gotten off to a slow start.
- Lack of planning at a federal level. For one thing, specific planning and details on vaccine administration didn’t emerge from the federal government and Operation Warp Speed until August of 2020. “In hindsight, it would have been better had it started earlier in terms of engaging state and local folks in the planning and readiness efforts,” Blumenstock said.
- Lack of resources into distributing the vaccine. He also said that while significant resources were made into developing and producing the vaccine, Operation Warp Speed didn’t make the same investments into distributing and administering it.
- Overpromise and underdeliver. Blumenstock said that similar to the H1N1 pandemic of 2009, this was a hard lesson to learn. There wasn’t enough managing of expectations and helping the general public understand how outlaying events could slow the pace of vaccine distribution and administration.
- Learning curve. Many of the challenges of vaccine deployment come from the fact that there is a learning curve with this vaccine and a need for an established cadence and predictability of supply. Furthermore, while states have existing immunization systems, a lot of them are navigating new systems and processes on the fly.
- What is success? Moreover, there still is uncertainty around what metrics are indicators of a successful distribution. “Is speed and volume a good metric to determine progress or success? Or is a metric that we don’t yet have, prioritizing risk and addressing equity, an equally good or better evaluation to use? Or is it both? That’s the tension we’re now experiencing,” Blumenstock said. He added that speed and volume may be less important than the ability to target high-risk individuals.
- Challenges in reporting. The data showing vaccines distributed is real time. The data showing vaccines administered has a few days lag. This is one reason there is a big delta between vaccines distributed and administered, Blumenstock said. There are also under-reporting challenges as providers figure out whether they should either get as many vaccines in arms as quickly as possible or catch up on the back-end process of reporting the vaccines administered. There is also a lack of interoperability, in some cases, between the state public reporting systems and a hospital’s EHR.
- Inventory management. States have been conservative with inventory management, Blumenstock said, because they aren’t sure when the second doses will arrive. There is a timing factor from when someone gets the first dose to when they need to get the second dose. Furthermore, states need to rebalance inventory in some cases because some sites are lower throughput. “Move inventory out of sites that aren’t seeing the clientele they anticipated and bring them into higher-volume sites that can readily apply that vaccine,” he said.
Vaccine hesitancy
As the U.S. improves efficiencies and operational challenges of deploying the vaccine, there will be other roadblocks going forward that will have to be addressed. One of the biggest issues going forward is vaccine hesitancy. A new survey from The Conference Board has revealed the scope of the problem facing health care leaders.
According to The Conference Board, 67 percent of these lower-ranking workers plan to take the vaccine. Of CEOs, 85 percent of those at the top plan to take it. “Indecision about the vaccine may be driven by a distrust of the health care system, government agencies, or the efficacy of the vaccine itself. In many states, the vaccination registration process can be complicated,” stated Amy Lui Abel, PhD, Vice President, Human Capital Research at The Conference Board. “Many companies, on the other hand, have the trust of their staff; they may consider sharing facts and dispelling myths about the vaccine, or enabling government plans to immunize their workers.”
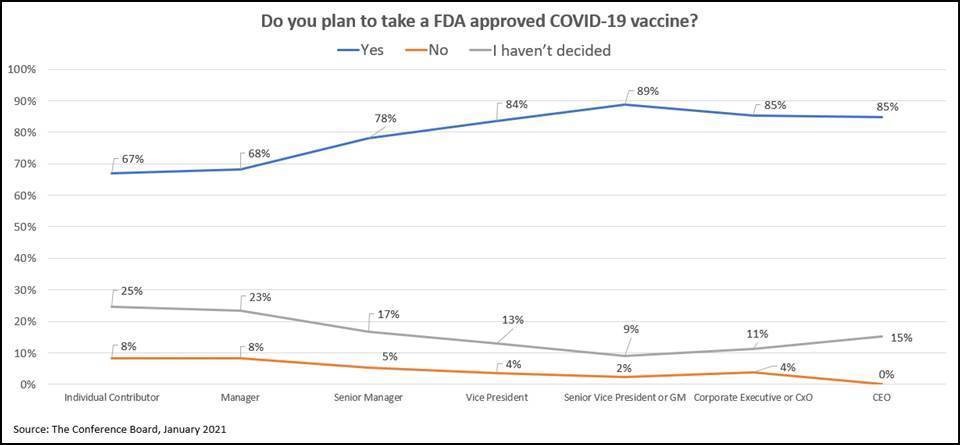
Data: The Conference Board
Addressing vaccine misinformation and improving hesitancy is imperative to ensuring vulnerable populations are getting access to the vaccine, said Kate Johnson, Program Director, Healthcare Cost and Coverage, National Governors Association, on the webcast with Blumenstock.
“Equity is critical. On the vaccine engagement front, that means you’re addressing things like different languages and cultural competencies in your communications. You’re using different modalities, ones that are more familiar to certain individuals. Inform your approaches by engaging with the community and tailoring those approaches as needed,” Johnson said. “And it’s not just about communication and hesitancy but make sure the access is there as well.”
Homepage image credit: Steven Cornfield/Unsplash










