The COVID-19 pandemic continues to ravage the country, with hospitalizations rising by at least 5 percent in 36 states and numbers reaching nearly 75,000 new cases and 534 deaths per day. Entering the traditional flu season with COVID-19 us still ongoing has the potential to make this latest wave worse.
“As we move into the fall and winter seasons, health systems must not only plan for the annual increase of influenza-related admissions, but also the increase in COVID-19 hospitalizations,” says Neil Carpenter, VP Strategic Planning of Array Analytics.
What will be challenging for hospitals is to plan for the unpredictable. Flu season tends to follow a predictable pattern in terms of hospitalizations, but COVID-19 has been anything but certain. To illustrate the challenges of this two converging illnesses, Array has overlayed the weekly hospitalizations rate per 100,000 during the first 30 weeks of the most recent flu season (2019-2020) with the most recent 30 weeks of the COVID-19 pandemic for a sample of four states (see above).
COVID-19 Innovation Guide: Returning to the Next Normal
What’s clear, Array says, is that the COVID-19 weekly hospitalizations are nearly three times higher than flu hospitalizations in some cases. Moreover, unlike the flu, COVID’s patterns are unpredictable because they rely on human behaviors (people following orders to stay home vs. people getting tired and going out) and differences in the nature of how the disease spreads (e.g. super spreader events and super spreader individuals).
Even with a “good” flu season with fewer hospitalizations (140,000 in the 2011-2012 season), hospital CEOs will have to be prepared to flex staff and manage capacity for triage and admission if COVID-19 hospitalizations continue to swing unpredictably. The combo of the two diseases could have a devastating impact on vulnerable adults, according to public health experts.
“It won’t take a ‘bad’ flu season—just ‘a’ flu season to make things more difficult in the ER and elsewhere in the US health care system,” said Nicholas F. Vasquez, MD, vice chair of the Diversity, Inclusion, and Health Equity Section of the American College of Emergency Physicians. “Further strain due to the co-circulation of flu and COVID-19 could disrupt routine care and have detrimental consequences for adults with chronic health conditions.”
According to the National Foundation for Infectious Diseases, 60 percent of American adults have one or more chronic health condition, including heart disease, lung disease, and diabetes, that put them at increased risk for flu and COVID-19. In particular, over the past eight US flu seasons, nearly 47 percent of patients hospitalized for flu had heart disease, making it the most common underlying health condition associated with flu-related complications.
What could make this even more challenging, is according to a recent survey by the foundation, is the fact that nearly 25 percent of American adults said they do not intend to get vaccinated during the 2019-2020 flu season. Thus, one of the biggest tasks for health care organizations this year, from a messaging standpoint, will be to ensure that everyone gets a flu shot, says NFID Medical Director William Schaffner, MD.
“While we currently don’t have an approved COVID-19 vaccine in the US, we know that annual flu vaccination can help protect these patients from hospitalization, progressive disability, and even death. It is imperative that health care professionals educate patients with chronic health conditions about their risks and implement strategies to increase flu vaccination rates during the COVID-19 pandemic,” says Schaffner.
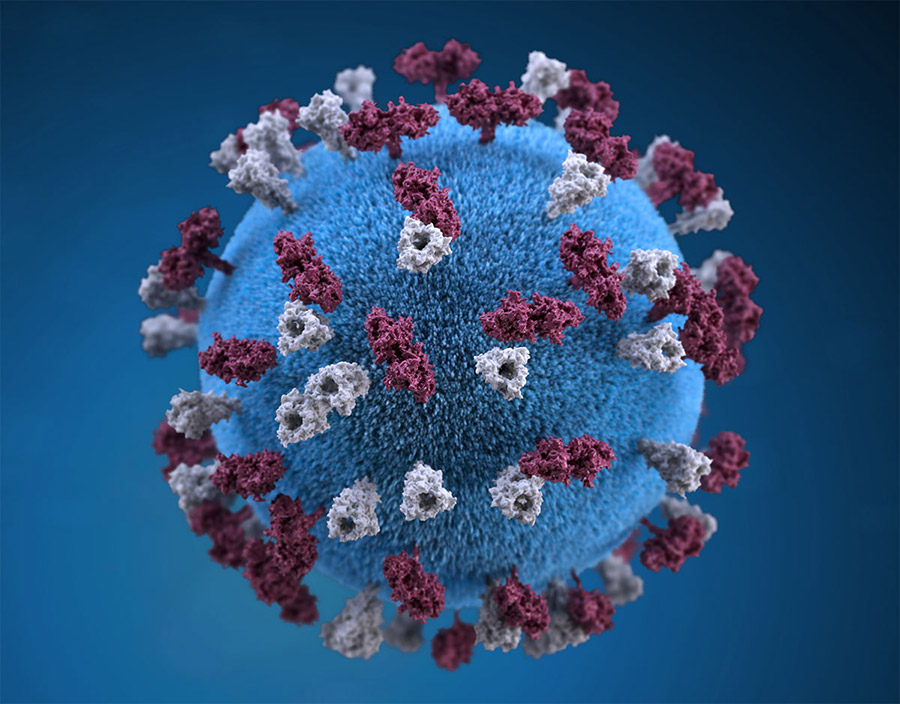
Homepage image credit: CDC