Mental health-related consults rose dramatically as the COVID-19 pandemic began. Now, as the nation prepares for what could become another surge in infections, some geographical regions are faring worse than others.
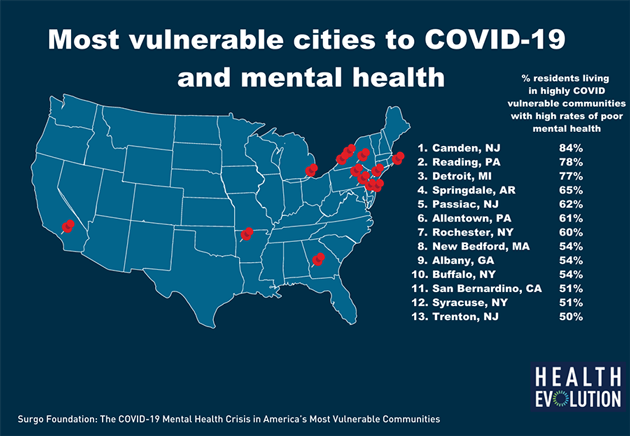
Surgo Foundation and Mental Health America joined forces to determine which U.S. cities are struggling the most with COVID-19 and mental health.
“These thirteen cities share one common, troubling characteristic: according to the CDC and the Surgo COVID-19 Community Vulnerability Index (CCVI), the majority of their residents live in neighborhoods that are both very vulnerable to the impacts of the pandemic, and have an extremely high rate of existing mental health conditions,” said Christine Campigotto, Program Manager at the Surgo Foundation.
COVID-19 Innovation Guide: Returning to the Next Normal
Here are the cities most vulnerable to COVID-19 and mental health issues:
-
- Camden, NJ
- Reading, PA
- Detroit, MI
- Springdale, AR
- Passaic, NJ
- Allentown, PA
- Rochester, NY
- New Bedford, MA
- Albany, GA
- Buffalo, NY
- San Bernardino, CA
- Syracuse, NY
- Trenton, NJ
Campigotto explained that Surgo’s CCVI aggregates a number of variables directly related to COVID-19, including socioeconomic status, population density, comorbidities as well as hospital factors, such as ICU bed availability. The Centers for Disease Control and Prevention’s “500 Cities” data set, meanwhile, consists of self-reported information about the percentage or residents with poor mental health.
“When we overlap these two datasets we can find unique areas where both of these risk factors overlap, creating a potential perfect storm for a mental health crisis as the impacts of the pandemic continue to worsen,” Campigotto said.
COVID-19 has also exacerbated existing inequities in health care and underlying disparities have made those worse.
Contact tracing: CEOs must remain vigilant on patient privacy
Surgo found that one out of every 1,000 people living in a vulnerable area has died from COVID-19 this year — which means that people in vulnerable areas are twice as likely to die than those in cities not on the list.
To address the underserved communities, Campigotto urged payer and provider CEOs to prioritize equitable allocation of mental health resources to communities in need and make telehealth mental health care services permanent and more broadly available. Additionally, she called on executives and public health leaders to support communities and individuals experiencing financial hardship, homelessness, lack of access to childcare or education to mitigate secondary impacts of the pandemic.
“Even after the pandemic has subsided, these communities — and many across the country — will continue to need increased access to comprehensive mental health care and a number of policy interventions to support them in getting their lives back on track,” Campigotto said.
Related articles:
Advancing innovative home-based chronic care management: Opportunities and obstacles
The 20 rural areas most vulnerable to COVID-19
‘Our health systems are not too big to fail,’ CEO warns