The financial ramifications of the pandemic on health care provider organizations have been well documented—but the clinical ramifications are less clear.
Clinical ramifications not just for those diagnosed with COVID-19, but for those who have avoided hospital treatment out of fear of the virus. The health debt crisis is one that could be impacting the health care industry for years, if not decades, to come.
Read more: Health debt: The next crisis for CEOs to anticipate
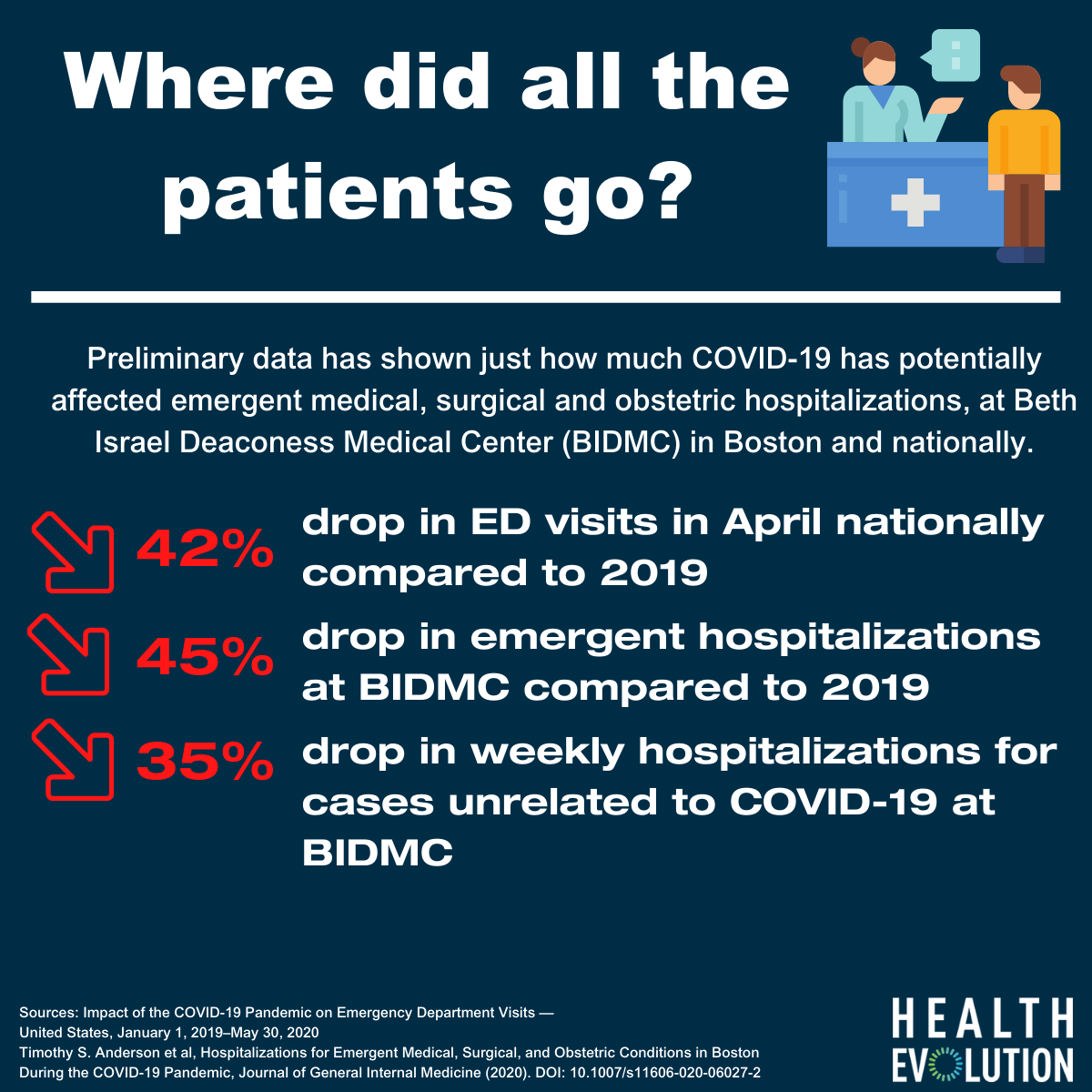
This week, Beth Israel Deaconess Medical Center (BIDMC) released some preliminary data on how COVID-19 has potentially affected emergent medical, surgical and obstetric hospitalizations. According to BIDMC’s data, there was a 35 percent decrease in weekly hospitalizations overall from mid-March 2020 to late April, when compared to the same period in 2019. For cases unrelated to COVID-19, there was a 45 percent decrease in weekly hospitalizations.
“Our findings suggest that patients with life-threatening conditions may have been avoiding the hospital in the early wave of COVID-19 which may help explain recent reports of increased mortality from diseases other than COVID-19 during this time,” stated Timothy Anderson, MD, general internist and health services researcher in the Division of General Medicine at BIDMC and Instructor in Medicine at Harvard Medical School. Anderson was the lead researcher on the study.
When analyzing the data against last year, Anderson and co. found a 51 percent decrease in hospitalizations for acute medical conditions, such as cardiac arrest or stroke; a 31 percent decrease in acute surgical conditions, such as appendicitis; a 55 percent decrease in chronic disease exacerbations, such as diabetes or asthma and 13 percent decrease in obstetric hospitalizations.
The researchers clarify that the reduction in hospitalizations could be because many college students in the Boston area left the city during mid-March. However, other data suggests that the fears are related to COVID-19. Nationally, in April, the CDC reported there was a 42 percent decline in year-over-year visits from 2.1 million per week in 2019 to 1.2 million per week in 2020.
A new survey of patients from the American Heart Association (AHA) reveals more than half of Hispanics (55 percent) would be scared to go to the hospital if they thought they were having a heart attack or stroke because they might get infected with COVID-19. The survey found that 45 percent of Black Americans feel the same way and 40 percent of white people.
The long-term impact of this pandemic on patients with chronic conditions, in particular, is something that health care CEOs are focused on. Cecelia Health CEO Dave Weingard told Health Evolution last month, “Without question, every day we need to treat people with chronic diseases such as heart health, obesity, diabetes, those are problems that need to be addressed. We have a second wave coming where patients who are not well–controlled in their chronic conditions have a high likelihood of complications.”