The COVID-19 pandemic has accelerated innovation in health care in ways that have never been seen before. The University of Pittsburgh Medical Center (UPMC) health system had 14,000 telehealth visits per day in the peak of March and April, which has since leveled off to 4,000. Two days in March alone matched the entire total of visits in all of 2019.
With a new baseline of telehealth established, health systems must begin to integrate the technology appropriately into care delivery, says UPMC CMIO Robert Bart, MD. “Telemedicine has had finally had its day and now that the genie is out of the bottle, as [CMS Administrator] Seema Verma, MD, said over the summer, it will be hard to put back in,” Bart said in an interview with Health Evolution.
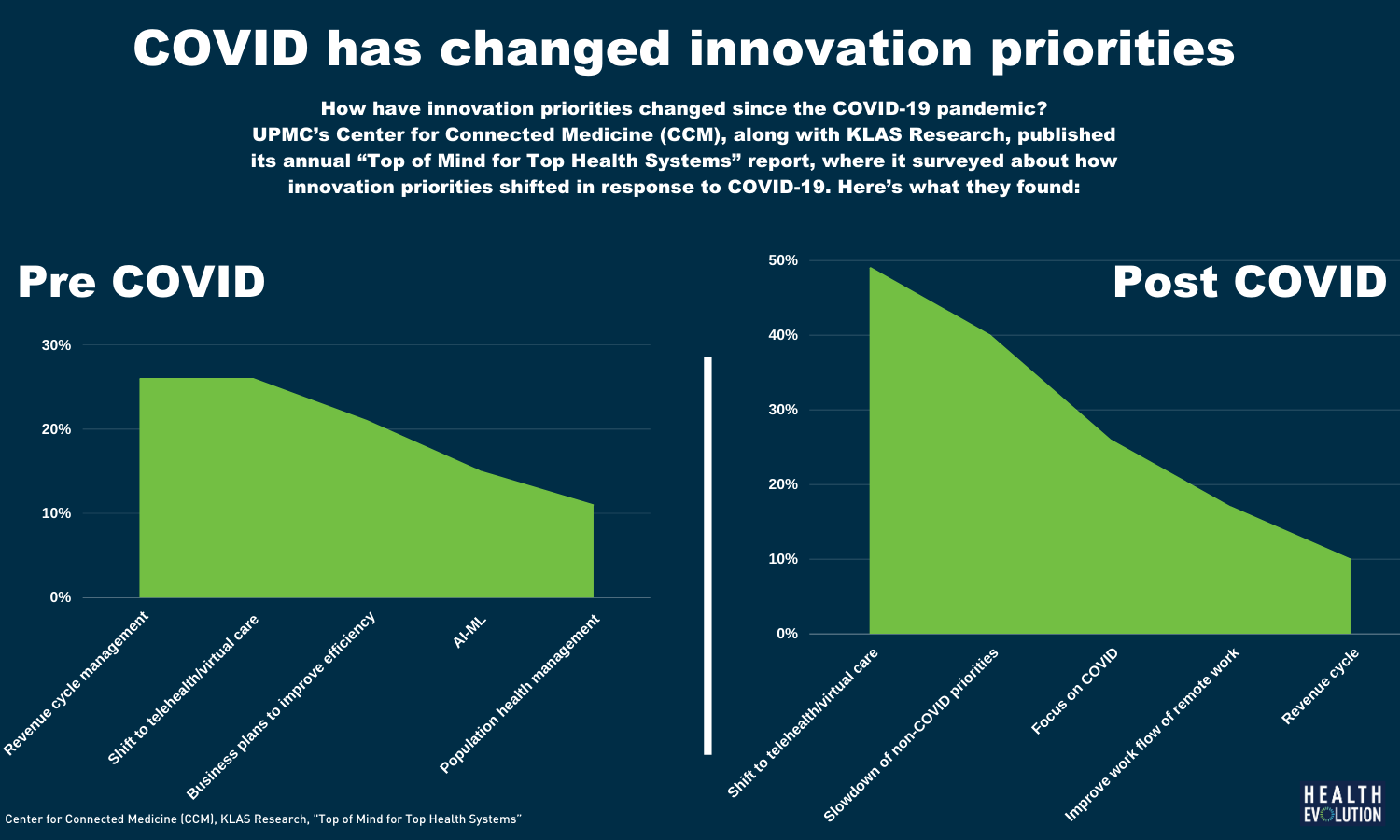
UPMC’s Center for Connected Medicine (CCM), along with KLAS Research, published its annual “Top of Mind for Top Health Systems” report, where it surveyed about how innovation priorities shifted in response to COVID-19.
Learn more about the Health Evolution Innovation Lab
The main findings reveal that while 91% organizations successfully met increased telehealth demand during the pandemic, quick implementation magnified opportunities for improvement, including integration and patient and clinician experience. Approximately 75 percent said their organizations are measuring and analyzing data from telehealth use to see how they can make it better going forward.
The report also touched upon how the pandemic forced health systems to innovate around the supply chain, put revenue cycle upgrades on the backburner and exposed their comfort level around AI. Bart spoke with us about some of the main findings of the survey and what CEOs can take away from it.
Health Evolution: What were the main results of this survey?
Bart: It’s not surprising that telehealth was a priority through the calendar year 2020 and will continue to be in 2021. Supply chain is rising to a level of importance as organizations are figuring out what is needed to take care of patients in this pandemic. That’s not something I would have thought would have risen to a level of importance, but having gone through the last six months, I recognize the importance of the supply chain and its necessity in this challenging time. Some of the things people have been traditionally focused on have had to be put on pause, relative to the pandemic. Previously, revenue cycle management and optimizing revenue opportunities was always something that was near the top of innovation priorities in most larger health organizations. That one certainly dropped—it’s dropped to number five since the pandemic.
Health Evolution: What surprised you?
Bart: The only thing is the recognition of the supply chain and its importance. I know I wouldn’t think of it. It’s extremely important. Part of UPMC’s success is related to the efficiency and effectiveness of our supply chain group. There’s an internal aspect of that. Organizations need to make sure their supply chain leadership, and those supporting it, have the right tools and right abilities to procure what’s needed for their health care workers and patients to be safe. But there is a larger component to that, from a regional and national aspect, which bore out in the early days of the pandemic. This speaks to us not having necessarily a good national infrastructure, or national decision making about the equitability of health care supplies during a pandemic.
Health Evolution: Based on this survey, what’s the next step for telehealth?
Bart: We have a new baseline in the amount of telemedicine we’re doing. We were doing on average 250 consumer facing telemedicine visits before the pandemic. At the peak of the pandemic, UPMC was doing around 14,000 per day. Now we’ve leveled off to around 4,000 per day. Four thousand per day has been quite consistent, so we have a new baseline. The opportunity is to now study how telemedicine can integrate into the appropriate care delivery for people who have different chronic diseases, chronic disease burdens, as well as acute disease management.
There was a forcing function in the early days of the pandemic where in many parts of the country, the only way you could get care was via telemedicine. Now we have safer ways of delivering face-to-face care. But we still see a persistently elevated delivery of telemedicine. Now we need to figure out what is the appropriate cadence of face to face and telemedicine visits in the ongoing management of patients, making sure the health care outcomes in telehealth are equivalent, as opposed to the traditional face to face.