It’s one thing when a large profit or non-profit health system, with money to invest in a strong virtual health program, can make a fast transformation in response to the pandemic.
Cleveland Clinic has taken a leading role transforming to a virtual care environment and sharing its digital playbook. Atrium Health in the Carolinas experienced staggering numbers in its shift to virtual care, to cite just two examples.
But what about safety-net hospitals?
Can a safety-net health system effectively switch to virtual care amid a pandemic, especially when you consider the fact they’re twice as likely to incur bad debt and pay for charity care than non–safety-net hospitals. Researchers at the David Geffen School of Medicine at UCLA have found that operating costs at a safety-net hospital are six times lower than non-safety-net hospitals.
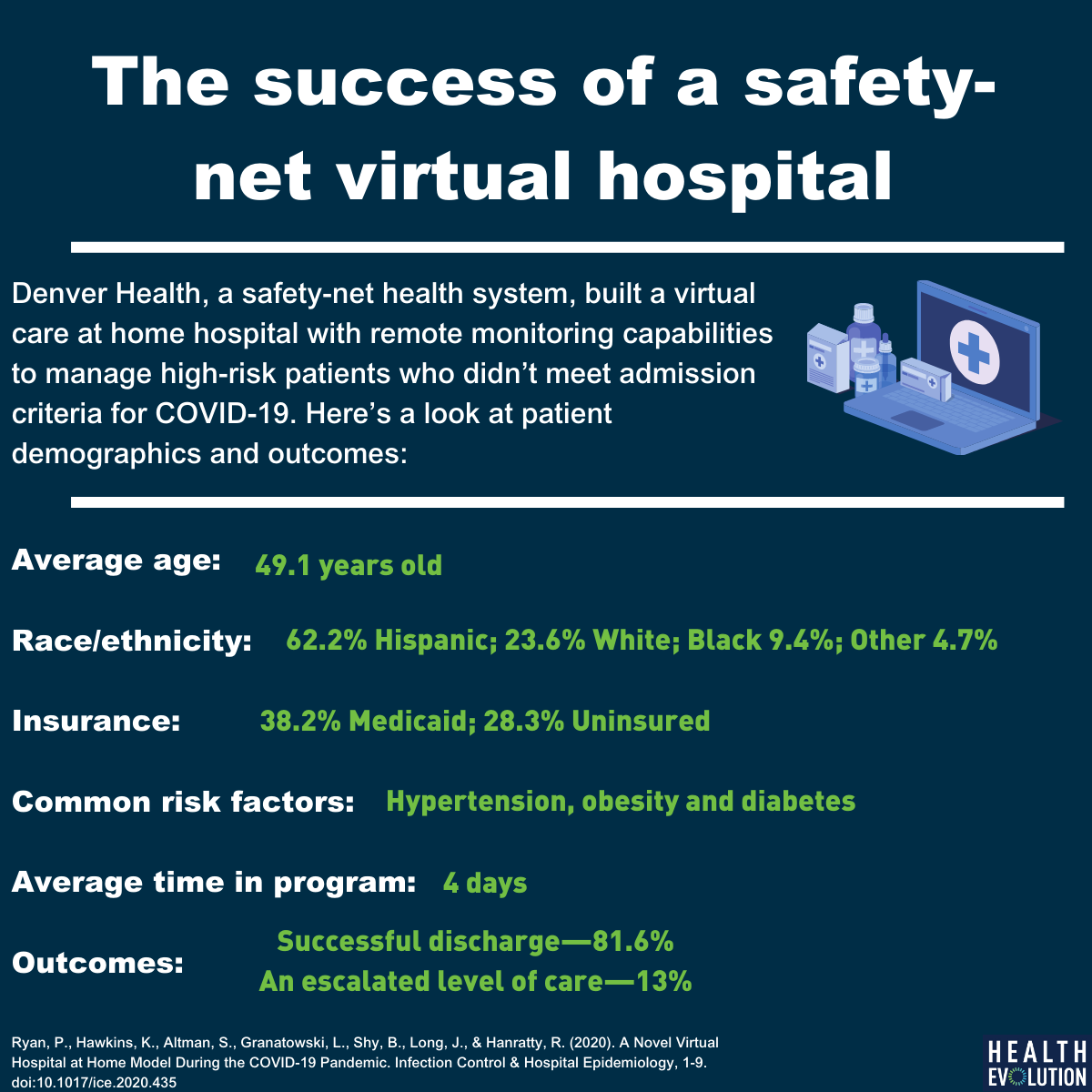
Denver Health, a safety-net health system in Colorado, is one of those organizations where the odds would seemingly be stacked against it succeeding in virtual care. The majority of its patient population on Medicaid (54%) or are uninsured (18%) and more than half are members of racial/ethnic minority groups.
However, by using its available resources in a pragmatic way, Denver Health built a successful virtual hospital at home program during the pandemic. After early experiences with patients discharged from the ED whose symptoms got worse, the health system provided care virtually to high-risk patients who didn’t meet admission criteria. The early results on its virtual hospital program are promising, according to a new study in Infection Control & Hospital Epidemiology.
“We weren’t developing new things. We were really leveraging what we’re already good at in terms of providing care in complicated situations. It came together because of that collaborative spirit,” says Jeremy Long, MD, who works in primary, urgent and complex care at Denver Health’s main campus and was one of the authors of the study.
The health system faced a challenge in acquiring enough pulse oximeter devices to send home with patients to monitor them remotely (along with automated blood pressure cuffs). Outside of that, the other necessary resources for the program included: Phone lines to make calls per day (one from a nurse and another from either a physician or advanced practice provider). interpreter lines, available clinicians, and a multi-stakeholder team that could help with operational challenges.
All of the above were at Denver Health’s disposal.
In the months of April and May, 233 patients were referred to the virtual hospital at home program. The average age was 49 and the most common risk factors were hypertension, obesity and diabetes. The average amount of time in the program for patients was four days. Of enrolled patients, more than 80 percent were successfully discharged from the program, 13.3% required an escalated level of care, and 5.6% percent were unable to connect. The majority of participants were either on Medicaid (38.2%) or were uninsured (28.3%).
“We developed something that was parsimonious. It was relatively simplistic, given available technology these days. We used simplistic means in a more sophisticated and pragmatic way,” Long says. “We didn’t have to go out and acquire a lot of extra technology. We used existing pieces and structures to meet a community need for people disproportionately impacted by this epidemic.”
The biggest potential roadblock? Not surprisingly, Long says, Denver Health had to be mindful of reimbursement around virtual care. As a safety-net institution with a number of federally qualified health centers (FQHCs), employees had to be careful about any new wrinkles added to a program, which included working in concert with the Colorado Medicaid program to clear up any potential challenges, Long says.
On top of its success in preventing a surge of patients from going into the hospital during COVID-19, the virtual hospital at home helped patients connect with enrollment services to implement medical coverage options and offered direct scheduling access into primary-care clinics. Immediate future plans for this program will be to keep it place during the COVID-19 pandemic, with potential opportunities to expand in the future to patients with chronic heart conditions, COPD, asthma, and diseases.
“I think it’s so critical to figure out who the stakeholders are in the process, identify both your clinical and non-clinical stakeholders. Recognize the more you do to enhance the communication and partnership of the siloed parts of health care—inpatient, emergency care, primary care—creating those relationships are the critical ingredients to make this helpful. We were lucky at Denver Health because we work hard to break down those siloes every day,” Long says.