The arrival of vaccines from Moderna and Pfizer may not come soon enough for a variety of reasons, not the least of which is the pandemic is having a damaging effect on patients’ mental health and overall wellbeing, according to new data.
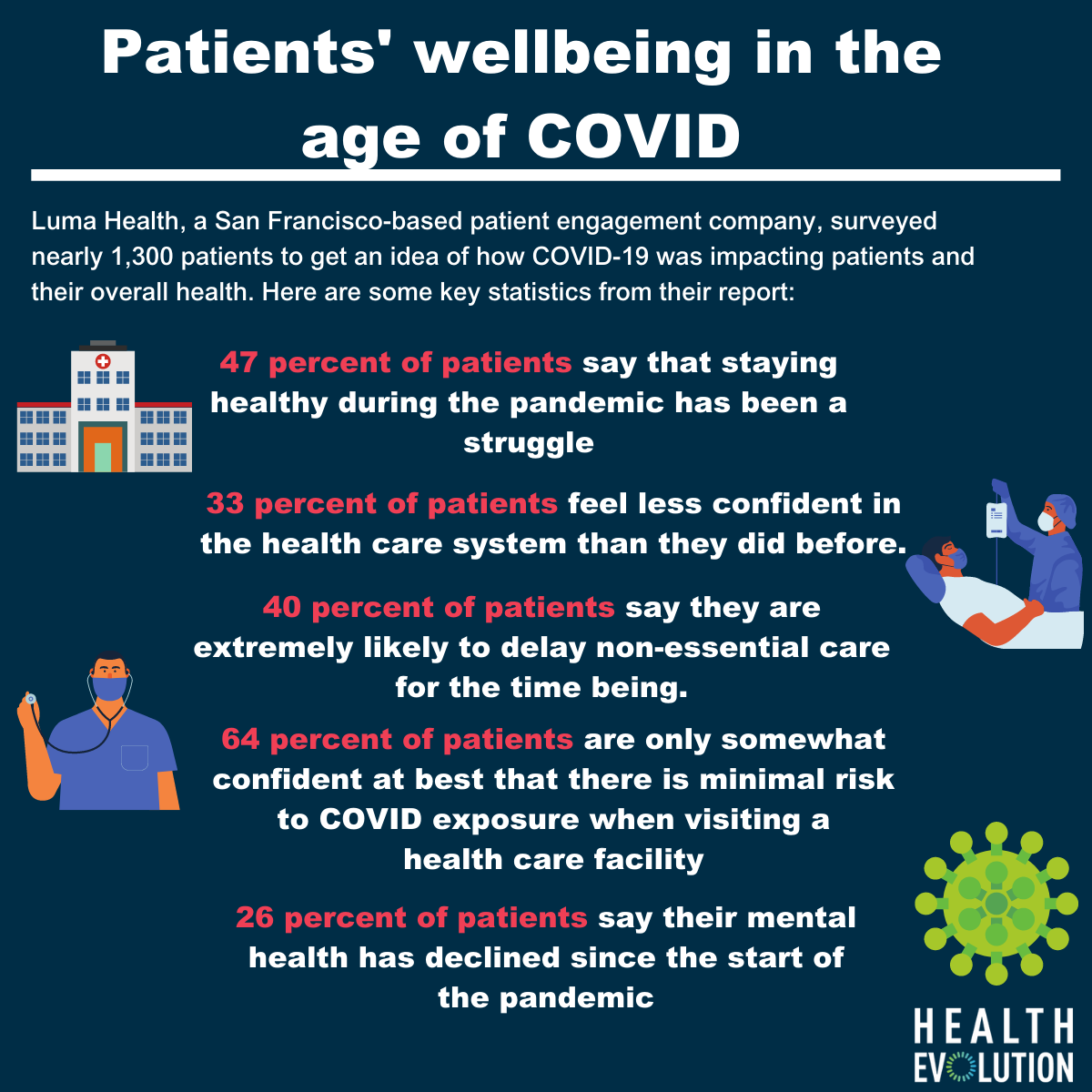
Luma Health, a San Francisco-based patient engagement company, surveyed nearly 1,300 patients to get an idea of how COVID-19 was impacting patients and their overall health. They found that 47 percent of patients say that staying healthy during this time has been a struggle and 33 percent feel less confident in the health care system than they did before. Even more alarming, 38 percent of patients say their health has been impacted because they are nervous about going to the doctor and potentially being exposed to COVID-19.
“During the second wave, we’re seeing patients are a little more comfortable in getting access to care even if it’s not an urgent issue. That said, a lot of patients are still afraid of going into their provider for a lot of their chronic issues. This fear, the inability to get direct access to their providers, is affecting their health,” says Tashfeen Ekram, MD, co-founder and CMO of Luma Health.
Luma’s survey found that a quarter of patients say their mental health has declined since the start of the pandemic. This finding jives with a survey of health care providers by researchers at the University of Leicester in the United Kingdom. That survey, which looked at the impact of COVID globally, revealed that 79 percent of providers say their patients’ mental health has worsened since the pandemic began.
Nearly two-thirds of patients surveyed by Luma are only somewhat confident at best that there is minimal risk to COVID exposure when visiting a health care facility. Nearly 20 percent of patients continue to cancel appointments based on these concerns and 40 percent say they are extremely likely to delay non-essential care for the time being.
In order to assuage these fears, provider organizations need to communicate better, says Ekram. Even though many provider organizations probably feel like they’re doing a sufficient job, he thinks that they can never go overboard in trying to get the message across that their hospitals and clinics are a safe place to go. They also should be regularly checking in with patients, especially those with chronic disease, who are feeling the pain of COVID-related disruption more than others.
“In some ways, chronic disease patients are afraid of getting access to care during the pandemic, but they welcome a shift in the way they interact with providers. They are interested in having a virtual interaction where providers would check their symptoms related to their chronic disease,” says Ekram.
More than 10 percent of patients with chronic disease say their condition has worsened during the pandemic, according to Luma’s data. The survey from University of Leicester found that diabetes (38 percent) was the condition reported to be most impacted by the reduction in health care resources due to COVID-19, followed by chronic obstructive pulmonary disease (9 percent), hypertension (8 percent), and heart disease (7 percent).
What’s more, a study in JAMA from researchers at NYU Grossman School of Medicine found “while hospitalizations for acute events began recovering in the late COVID-19 period, many of those related to chronic diseases generally did not.” The NYU researchers say the implications of these chronic disease patients not obtaining necessary hospital care are incredibly concerning.
Beyond patients with chronic disease, there is a sharp drop in childhood immunizations, say Ekram. In fact researchers at the CDC looked at orders for all routine non-influenza childhood vaccines for the period of January 6 through April 20 of this year to January 7 through April 21 in 2019. There was a decline of approximately 2.5 million doses from last year. In July, the World Health Organization and UNICEF warned of an alarming decline in the number of children receiving life-saving vaccines around the world.
The downside impact of these delayed services is that 40 percent of providers surveyed by Luma say they expect to see care disruptions and appointment cancellations related to COVID-19 for the next year or more. The arrival of a vaccine, however, could not come soon enough.
“We’re seeing a lot of these preventative types of care services, like immunizations, not happening right now. And the ones that are really hurting are the small to mid-sized practices that are having a hard time figuring out how to fix that gap,” Ekram says. “A lot of these physicians in these practices are concerned and not sure they’ll be open in the next six months.”
(homepage image credit: halfpoint/canva.com)