The Affordable Care Act saw a record number of enrollments for 2022. According to data from HHS, more than 14 million people enrolled ahead of the January 15th deadline, which beat out the previous record that was set in 2016.
The subsidies from the American Rescue Plan were a boon for the ACA signups. The law increased ACA marketplace subsidies above 400 percent of the poverty level and also increases subsidies for those making between 100 percent and 400 percent of the poverty level, for two years (2021 and 2022).
“This did not happen by accident. The American Rescue Plan did more to lower costs and expand access to health care than any action since the passage of the Affordable Care Act. It made quality coverage more affordable than ever—with families saving an average of $2,400 on their annual premiums, and four out of five consumers finding quality coverage for under $10 a month. As a result, millions of our fellow Americans have now gained the security and peace of mind that dependable health insurance brings,” President Joseph R. Biden Jr. said in a recent statement.
With more people enrolling in ACA plans, there are more insurers issuing plans. From 2020 to 2021, it went from 10,289 plants to 13,596. This year it’s up to 15,638. The peak was around 18,000 during the first year after the ACA passed.
The number of exchange offerings have grown 20 percent versus 6.8 percent for off-exchange only plans, according to analysis from the Robert Wood Johnson Foundation. Off-market plans, which are sold outside the marketplaces, are growing primarily on the backs of companies like Oscar and Bright Health. For Centene, UnitedHealth, Cigna, and Anthem, RWJF, there were few or no off-exchange plans added for this year.
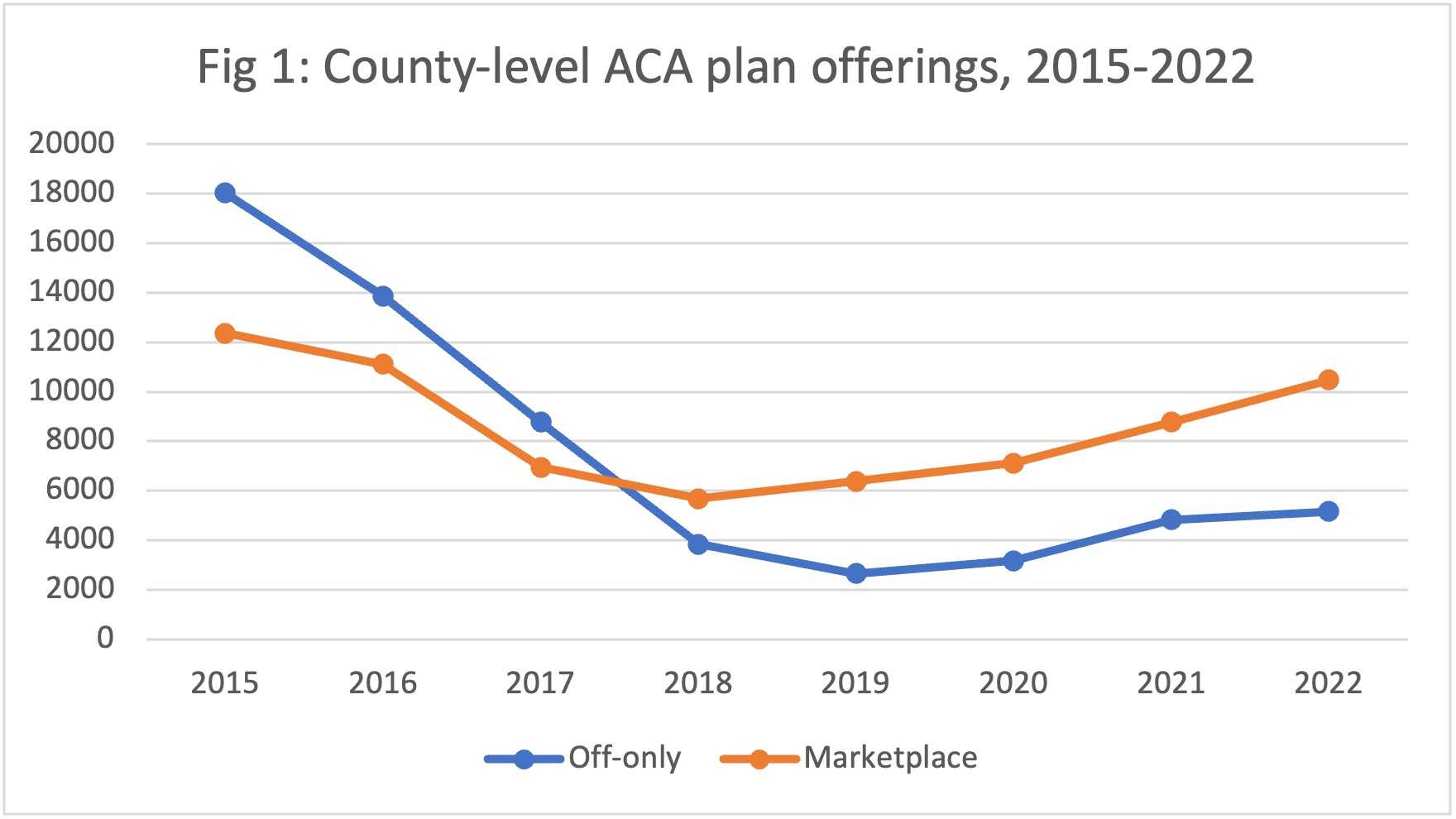
Credit: RWJF
For 2022, there have been additional plans added by Ascension, which added plans in Kansas (Wichita area), Michigan (Detroit area) and 30 counties in Indiana; CVS/Aetna, which returned to the ACA and offered plans in Arizona, Florida, Georgia, Missouri, Nevada, North Carolina, Texas, and Virginia; Oscar Health; which added plans in Nebraska, and also participated in co-branded “Cigna+Oscar” plans in Missouri, Kansas, and Tennessee.
“We anticipate our co-branded CVS Aetna offering and benefit design focused on consumer choice will result in gains of at least 100,000 new members in 2022,” said CVS Health CEO Karen Lynch on a recent earnings call.
ACA states that didn’t expand Medicaid saw the largest increases of overall enrollment growth, according to the RWJF analysis. Moreover, non-expansion states, such as Georgia and North Carolina, are top destinations for plans that are entering new states or expanding their footprint. Chini Krishnan, Co-Founder and CEO of GetInsured, which has a cloud-based easy-to-navigate health insurance platforms for state, says that the ACA has been remarkably resilient.
“States have continued to embrace the process of building out state-based marketplaces and exchanges and continuing evolution around getting network adequacy,” says Krishnan. “The broader story is that when you take the politics out of the picture and sort of look at the underlying trends, there is remarkable stability in ACA markets, remarkable entry of new carriers in the ACA markets, and in the wake of COVID, significant enrollment growth.”









