A hard truth emerging from the COVID-19 pandemic: Health care, at both a system- and organizational-level, must prepare more thoroughly for future outbreaks.
“The problem is [pandemics] happen with enough infrequency that every generation forgets the impact,” said Mike Leavitt, founder of Leavitt Partners and former HHS Secretary and Utah Governor. “The way to move through uncertainty is to create a list of assumptions that are directionally correct and then iterate.”
During the recent Health Evolution Pandemic Response: A Public-Private Call to Action webcast CEOs, policy makers and other leading executives discussed some aspects of the pandemic they are paying particular attention to now to ultimately apply those lessons to future outbreaks.
The following takeaways emerged from the half-day of discussions:
-
- Prepare for a second wave of infections
- Establish surveillance networks
- Improve management of PPE and other supplies
- Plan for earlier interventions in future outbreaks
- Reevaluate federal policy and public health
Executives explained why each of those is important now and moving into the future.
Prepare now for a second wave of infections
It’s too early to identify when the first wave will peak or decline exactly, or when COVID-19 could reemerge and set in motion another spread of infections, but executives are anticipating how to be more effective when that next wave arrives, possibly in the fall, based on lessons already learned.
FDA Principal Deputy Commissioner Amy Abernethy, MD, said the health care system will better understand how to put mitigation countermeasures in place, be smarter about population-based immunity and allocate care more effectively for very sick individuals. Another part of the response will be more testing than in the early stages.
“We’re still going to be trying to figure out the waxing and waning of disease to be sure we are managing the viral illness and make sure we have adequate health care available and make sure we’re ready to conduct an appropriate clinical trial,” Abernethy said.
Illumina CEO Francis deSouza added that the U.S. can monitor and learn from China and South Korea about removing sheltering-in-place restrictions to better understand what works and what does not.
Establish surveillance networks
While the spirit of collaboration between health communities and academic researchers around the world has been generally good, COVID-19 was “a big eye-opening moment,” about the need for more effective surveillance, deSouza said.
“We need to identify an outbreak when it’s happening, quickly characterize the outbreak, characterize the pathogen causing the outbreak, so we need surveillance networks,” deSouza added. “We thought we kind of generally had it, but this shows that we don’t. We don’t have a central surveillance network around the world.”
Klasko, Khosla look at the future of AI in health care post COVID-19
Abernethy agreed that health care is not as mature in surveillance capabilities as many would like and added that organizations also need to have data systems ready for rapid analysis during emergencies.
“We want to essentially widen the aperture of our systems quickly for situations like this in the future,” Abernethy said.
deSouza pointed to UCSF and Stanford as being among the organizations undertaking enormous cooperation in sharing tools and learnings. Most efforts are currently happening on a regional basis, so the next step will be to connect those surveillance networks.
“We need at least a national if not an international approach to pandemics. An outbreak in a fish market matters to all of us. Pulling inward and distancing yourself from the rest of the world is a mistake. It matters what happens in Africa, it matters what happens in Asia,” deSouza said.
Improve management of PPE and other supplies
COVID-19 has put considerable stress on health care organizations’ ability to procure supplies as demand surged for medications, ventilators, PPE, swabs, reagents, drugs needed for intubation, and more.
While the private sector has stepped in, such as automobile manufacturers producing masks, even that is problematic as components are imported from around the world, said Julie Gerberding, MD, Executive Vice President & Chief Patient Officer at Merck. Obtaining even basic equipment can take a prohibitively long time.
“We are highly interdependent on a global basis for the various components of our support,” Gerberding said. “It’s demonstrating the connectivity of our supply chain.”
What’s more, the U.S. Strategic National Stockpile essentially dried up by the second week of April with reports indicating that 90 percent of the stockpile’s PPE has been distributed by April 8, 2020.
“I hope a lesson is that we truly federalize the approach to PPE management because there’s unevenness across the country,” said Mark Laret, CEO of UCSF Medical Center. AdventHealth CEO Terry Shaw added: “I think the supply chain disruption and the ability to only get something from one place in the country or the world is going to change dramatically as we think about supply chain on a go-forward basis.”
Plan for earlier intervention in the future
The need to respond quickly in any emergency is not surprising. COVID-19, in fact, has resurrected this lesson from starkly different reactions to the 1918 flu in the cities of Philadelphia and St. Louis. Despite the outbreak, the former held a parade that caused approximately 2,600 deaths and the latter put in place measures to reduce public gatherings that resulted in a death rate estimated to be one-eighth of Philadelphia’s.
“The importance of early intervention has just been brought to the front,” Laret said.
In 2020, the San Francisco area began sheltering-in-place on March 16, the day before St. Patrick’s Day, and that move slowed the growth curve considerably more than even Southern California, Laret said.
Reevaluate policy and public health
The federal government made sweeping policy changes amid the pandemic, notably easing HIPAA, enabling clinicians to practice across state lines and reimbursing for telehealth or virtual visits, even when doctors use consumer apps such as FaceTime or Skype. Many people in the health care industry have spent years advocating for those changes with little more than incremental progress and policy makers instituted them in a matter of weeks responding to COVID-19.
Whether the government will revert to prior rules and regulations, leave some of the waivers in place, or begin fresh conversations about how to proceed when this particular coronavirus is under control remains an open question.
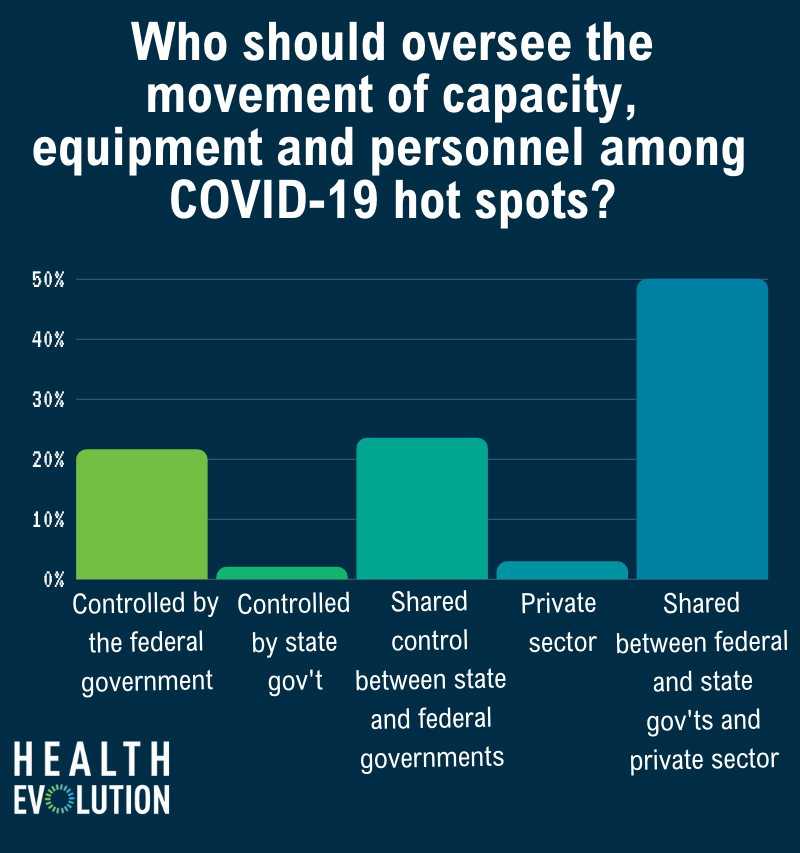
One thing that was clear among our webcast participants, however, is the need for private and public collaboration. We asked the polling question: Who should oversee the movement of capacity, equipment and personnel among hot spots?
Fifty percent of the 102 respondents to our poll said it should be shared between the private sector and federal and state governments, followed by the 24 percent indicating state and federal agencies, 22 percent saying the federal government alone, 3 percent opting for the private sector alone and 2 percent favoring state governments assume the responsibility.
“I hope that the world now understands how important it is to take care of communities and how public health matters more than anything we’re doing so that people have food and people have housing and people have literacy and kids aren’t subject to adverse childhood events,” said David Feinberg, MD, Vice President of Google Health. “Those are the drivers of really high health care costs and we keep having a system that’s been focused on that instead of moving upstream. And this is as upstream as it gets.”
COVID-19: A letter to America’s courageous clinicians
Leavitt, the former HHS Secretary and Utah Governor, envisions the data public health provides becoming a part of individual’s day-to-day lives. Much like checking the weather, people will check a virus report before traveling to a specific region and, in the event of rising COVID-19 levels, amend travel plans accordingly — the same way one might adjust a trip when there is a major snowstorm in the forecast.
Conclusion
Executives agreed that the U.S. health care system, and the world for that matter, will survive COVID-19. But the world has already suffered some losses and those will unfortunately continue into the future.
“We could have done much better and we need to hold ourselves to a higher bar because there will be a next pandemic,” Illumina’s deSouza said. “We can do much better going forward. We’ll move as fast as we can to get through this as quickly as we can.”
The learning curve to achieve better outcomes in the next pandemic — whether it happens again in this generation or the next — will inevitably be steep.
“There’s a to-do list of lessons learned that I’m keeping,” said Larry Jameson, MD, Dean of the Perelman School of Medicine, University of Pennsylvania, “to think about not only how we use these lessons the next time we have a pandemic but, more importantly, how do we use them to make our health system better in the future across the board?”
Related:
How CVS Health, Teladoc and Google Health view consumerism during COVID-19
On Demand: Health Evolution 2020 Pandemic Response Virtual Gathering
Health care leaders share biggest hopes and fears amid COVID-19










