Jim Albin, CIO of Thedacare
As health systems, hospitals and practices build out population health strategies and increasingly serve urban and rural communities, they must optimize new care modalities to engage people in different geographic areas.
“It’s one thing to serve patients in an urban area like Appleton, but it’s a completely other thing to be in a rural environment. Rural households are busy taking care of their farms. They don’t have time to take a three-hour round trip to see the doctor or hop on the phone for two hours,” says Jim Albin, chief information officer, Thedacare, in Appleton, Wisconsin. “We want to be available to that rural household to allow them to interact with a sophisticated health system so they are reassured of [their health status] and if something pops up, we can recommend that they come in.”
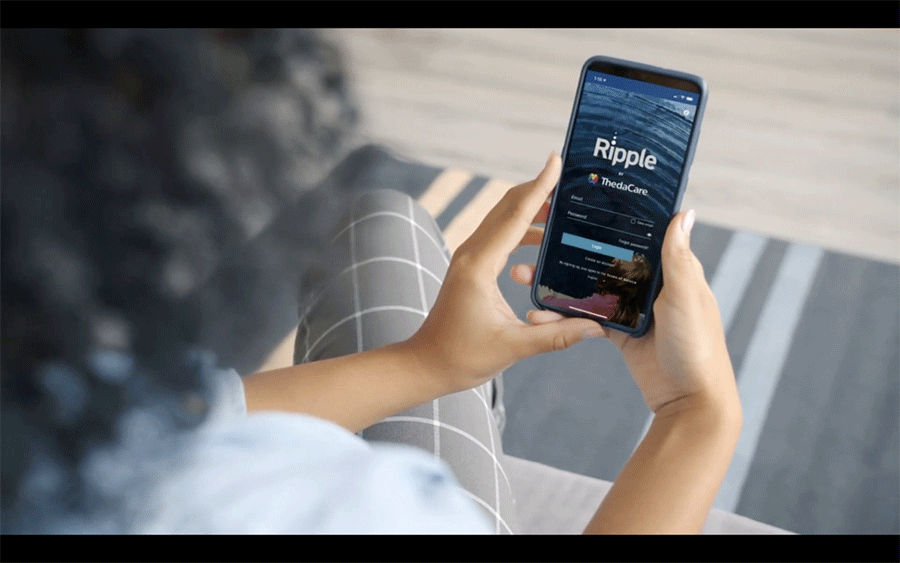
For Thedacare, getting patients throughout northeast and central Wisconsin to engage with their health care can be a challenge regardless of the circumstance and location, but that’s especially true when there’s a pandemic that forced people to stay home. To achieve that, ThedaCare last year took an investment stake in startup b.Well Connected Health and the two have since jointly built a digital health app called Ripple.
The app aims to coordinate a patient’s health information across different providers, pharmacies and other sources. ThedaCare uses Ripple to inform patients about their own health status, access their provider and insurance information, manage medications, schedule visits, and receive alerts on future care needs. Moreover, the app has served as a way to educate people on COVID amid a flurry of misinformation on the disease.
The overall goal, Albin says, is to become a “household standard” the same way that other apps are used to track, for example, someone’s personal finances. “At the end of the day, we’ve been through the phone trees and all those kinds of things. “When patients are feeling sick, who wants to go through a six-level phone tree to actually talk to someone? You’d rather pick up your phone, make a few clicks and know that you can make an appointment,” he says. “Everyone is so used to being digital. How many places even work with cash anymore? It’s all electronic and this will be another aspect of that.”
Thus far, ThedaCare has seen success with Ripple. At a recent conference, CEO Imran Andrabi said 83 percent of the system’s high-risk individuals have downloaded and are interacting with the app in meaningful way, 67 percent of population at ThedaCare are using Ripple and the number of people who signed up for app is up by 312 percent over last 10 months.
The challenge of interoperability
What’s thwarted these kinds of apps in the past has been a lack of interoperability and a siloed health system. Albin says health information exchanges have been inhibited by the lack of national patient identifier.
In this area, b.Well and Mastercard are teaming together to create a digital ID verification tool for health care organizations that uses facial biometric technology. ThedaCare will be one of the first users of the tool. Albin says this method goes beyond any traditional avenues of identity security seen in health care. “What can be more secure than the uniqueness of a person’s appearance or biometric background?”
But the challenges of interoperability go beyond issues around patient identity. As Albin notes, patients typically have multiple portals for the different points of entry within the health care system and various stakeholders haven’t always been eager to share. All told, interoperability has been the health care industry’s white whale for quite some time.
“EMR vendors always thought they were the center of the universe. They would have open arms for anyone to send them information but no inclination to send any information back out there. That’s why best of breed died,” says Albin. Those challenges still exist but the regulations coming out of the 21st Century Cures Act, the emergence of the Fast Healthcare Interoperability Resources (FHIR) standard, and other pushes from the industry are starting to make a difference, he says.
“There is an expectation and recognition by the government that this information needs to flow freely. You can’t hold information and try to use it as a leverage for your business,” Albin adds. “It has to be patient focused. Patients need to have the full picture of what’s going on and nothing is getting held back.”
This will be a big change in the years to come, but it won’t be spurred by the government alone. As health care moves into a more population health mindset, Albin says industry leaders need to recognize that one vendor cannot possibly serve all their different constituents. Therefore, health care leaders will need to take an active role in finding and connecting the best software applications to engage their patients.
“Be open minded. Recognize you have to manage it because you can’t have 17 different vendors running around. Recognize that each one of these tools will have a place in the bigger picture. If you stay with one or two vendors, will it work? Maybe. Will it be an optimum situation? Maybe not. These tools focus on different parts of the continuum of care and no one vendor can provide it all,” says Albin.
Homepage photo credit: b.Well Connected Health/ThedaCare