The Issue: Although data around vaccine distribution in America is sorely limited and scattered, one pattern is becoming increasingly clear – those who have been affected by COVID-19 the most are getting vaccinated the least. Based on early data from 26 states, Black and Hispanic Americans are getting vaccinated at approximately half and one-third the rate of white Americans respectively, even after controlling for the demographic makeup of health care workers. Meanwhile, Black, Indigenous, and (other) people of color (“BIPOC”) are contracting COVID-19 at nearly twice the rate, being hospitalized for COVID-19 at nearly four times the rate, and dying from COVID-19 at nearly three times the rate as white Americans.
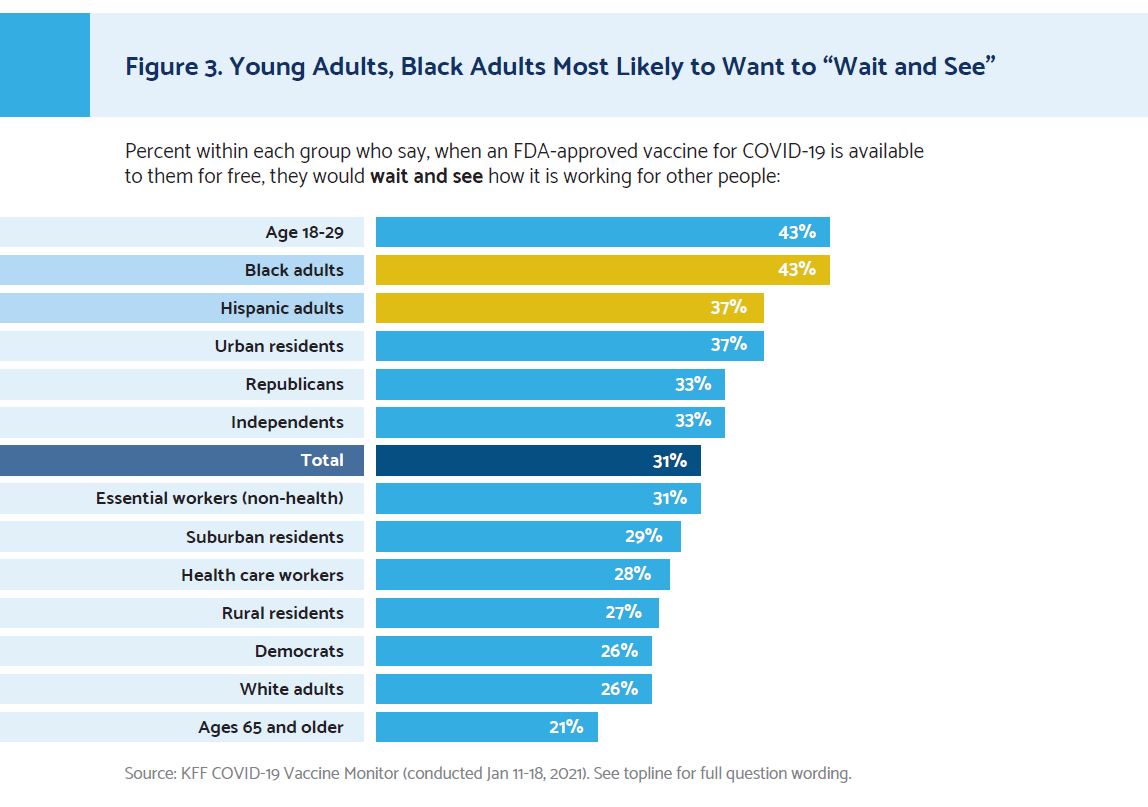
Disparities in vaccine uptake stem from both lower confidence in and less access to the COVID-19 vaccination. First, many individuals in diverse communities are less confident than white Americans in the vaccine, with 43% of Black adults and 37% of Hispanic adults stating they would “wait and see” how it is working for others before getting it. Second, vaccine distribution is commonly done in ways that are less accessible to BIPOC Americans in both obvious ways (e.g., distribution sites are placed farther from BIPOC communities), and more subtle ways (e.g., accessing the vaccine requires an individual to have resources—time, transportation, computer and Internet access, knowledge of how to get vaccinated, etc.—that are not equitably distributed by race and ethnicity).
10 Recommendations: Health care CEOs are in a unique position to increase confidence in, and accessibility to, the COVID-19 vaccine. Fixing the deep inequities embedded in the health care system is beyond the scope of this guide, but CEOs can take the following 10 steps today to increase vaccine confidence and accessibility in the diverse communities they serve:
PART I: Creating an Action Plan
- Step 1: Empower a Task Force to Provide Oversight
- Step 2: Coordinate with Community Organizations and Local
- Government
- Step 3: Conduct a Rapid Root Cause Diagnostic
PART II: Increasing Confidence
- Step 4: Identify and Train Trusted Messengers
- Step 5: Be Transparent About Vaccine, Allocation, and Distribution
- Step 6: Create Personal Messaging
- Step 7: Use Evidence-Based Messaging
- Step 8: Communicate Through Multiple Touchpoints Consistently
PART III: Increasing Accessibility
- Step 9: Make Signups as Accessible as Possible
- Step 10: Distribute the Vaccines in Local Places
About this Guide: This document was developed by Fellows on the Roundtable on Community Health and Advancing Health Equity, with support from Health Evolution staff and Benjamin Bolnick and with significant input from both the Work Group on Building Scalable Models and Community Partnerships to Address Social Determinants of Health and the Work Group on Leveraging Data to Improve Health Equity. This working guide is available to the public on a webpage with commenting functionality. New versions will be released to respond to feedback received and to the emergence of additional data and best practices.